Save to my favorites
What is it?
With “direct to implant” reconstruction, the surgeon reconstructs your breast in a single step, placing the saline or silicone implant in one operation. Unlike traditional implant reconstruction, this procedure does not use a tissue expander.
Learn more about direct to implant reconstruction:
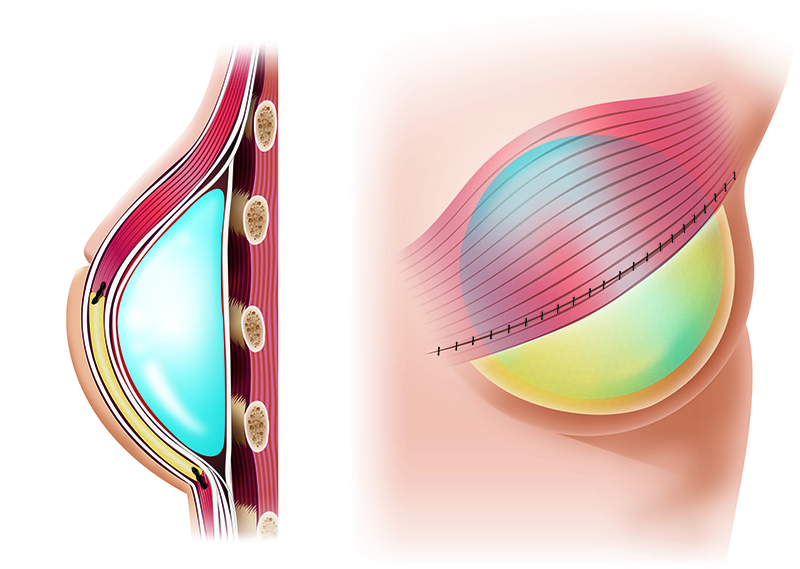
In direct to implant reconstruction, the surgeon puts saline or silicone implant under your chest skin and muscle to create the breast mound. Generally, this approach is possible only for immediate reconstruction (reconstruction performed at the time of the mastectomy).
This technique is possible only with a skin-sparing or nipple-sparing mastectomy, because enough extra breast skin must remain after the mastectomy to cover the implant.
If there is not enough remaining skin to allow for immediate placement of a full implant, the surgeon likely will place a tissue expander instead. This allows for growth of additional skin and for placement of a saline or silicone implant at a later surgery. (See expander-implant reconstruction).
The direct to implant technique usually uses a piece of banked human skin to create the inner shape of the new breast. This skin has been:
- Harvested from human donors
- Radiated to prevent rejection
- Sterilized to reduce chances for infection
The donor skin is sewn into the implant pocket to keep the implant centered and to maintain the proper shape.
Implants
- Have round or teardrop shapes and covers made of silicone plastic
- Are filled with silicone gel or saline
- Silicone: a semi-solid gel
- Saline (Salt water)
Learn more about silicone versus saline implants:
Silicone implants
- Usually filled with thick, compressible silicone gel
- Usually feel softer and feel more “natural” than saline filled implants
- Less likely to show visible “wrinkling” or “rippling” on the skin surface, compared with saline implants
- If you had an implant leak, you might not be able to see or feel it, and you would probably need breast imaging (an MRI scan) to find the leak
Saline Implants
- Filled with saline (salt water)
- More likely to show visible “wrinkling” or “rippling” on the skin surface than silicone implants
- May have a firmer feel, compared with silicone implants
- If you had an implant leak, the implant will deflate and look flatter, so you would not need breast imaging to find the leak
How is it done?
The surgeon places the implant under the chest muscle and remaining breast skin, typically through the original mastectomy incision, to help create the shape of a breast.
Learn more about the steps
Start
Implant Placement
- Done at the same time as your mastectomy or later
- Takes about 2 to 3 hours
3 Months
Nipple Reconstruction or other optional procedures
By the numbers
- Number of surgeries:1 (usually)
Patients who have this type of reconstruction generally need 1 surgery:2 - 3 hour surgery to place the implant, depending on whether one or two sides are being createdThe implant surgery is combined with the mastectomy (“immediate reconstruction”).
- Nights in the hospital:0 or 1
This surgery may require at most 1 night in the hospital.
- Length of recovery:3 to 4 weeks
Recovery times vary, but you can usually go back to normal activities, including driving, after 3 to 4 weeks.Even after the initial recovery time has passed, you still may not feel like yourself. You may still feel tired and sore for a few months after your surgeries.
What are the pros?
- Shorter surgery I Little or no hospital stay
The surgery to place the implant is shorter (2 - 3 hours) when compared to other reconstruction options.If you choose to have reconstruction during your mastectomy, you will likely stay in the hospital overnight after the combined mastectomy and breast implant placement.
- Faster recovery
Because implants require less extensive surgery than other reconstruction options, usually less recovery time is necessary.
- Less invasive | Fewer scars
Since no tissue needs to be taken from other areas on your body with this approach, implant surgery leaves fewer scars. In most cases, the mastectomy scar (or incision) is used to place the implant, so you will have no extra scars after the reconstruction.
- Good cosmetic results for most women
Implant reconstruction on one breast with adjustments to the opposite breast generally has good cosmetic results.
What are the cons?
- Harder to match opposite breast
Implant reconstructions offer less flexibility in creating shapes to match your opposite natural breast. Unlike natural tissue flaps, implants cannot be sculpted to customize their shapes.As a result, you may want changes to the opposite, natural breast so it matches the implant more closely.Implants also may not feel completely natural to the touch.
- May not “sag” naturally to match the opposite breast
Implant-reconstructed breasts tend to have “youthful” shapes, that is, very little sag, and the shape usually does not change over time. Natural breasts will likely droop (sag) with age.Patients with implant reconstruction on one side may not stay symmetric (or even) over time, compared to the opposite, natural breast. You might need more surgery on the natural breast to re-establish symmetry later in life.
- Implants won’t change in size with body weight gain or loss
Implants do not change in size or shape to match changes in body weight. This means that the size and shape of your implant-reconstructed breasts will also remain the same, regardless of changes that may occur elsewhere in your body. If you lose or gain weight, your breasts may seem the wrong size compared to your new body shape.
What are the risks?
- Infection
- About 10% of patients (1 out of 10) will get an infection after the implant surgery. This can require a hospital visit or another surgery. Sometimes the doctor has to remove the implant because of infection.
- Bleeding or fluid collection
- 2% of patients (2 out of 100) may have bleeding (“hematoma”) or fluid collection (“seroma”) under the breast skin after these surgeries. Although not life threatening, this may mean a hospital visit or another surgery.
Possible long term problems
- Leakage of the implant
- The most common complication of implant reconstruction is leakage. This happens in about 10% of patients (1 out of 10) over the first 10 years for either saline or gel-filled implants. At this time, there are no reliable data that track an implant after the first 10 years.
When leakage occurs, the implant must be removed or replaced. This procedure usually takes about an hour and does not require a hospital stay. For silicone gel implants, more extensive surgery is sometimes needed to remove loose silicone from the breast area. However, this tends to be less of a problem for the newer solid or semi-solid silicone gel implants.
- Pain from scar tissue
- Scar tissue forms on the outside of all artificial devices (like implants) when placed in the body. Usually, this does not pose a problem. However, in about 5 to 10% of patients (5 to 10 women out of 100), too much scar tissue forms. This may happen more frequently with silicone implants than with saline implants. The scar tissue may cause pain and discomfort and make the implant feel hard to the touch.
If this happens, you may need surgery to break up or remove the scar tissue. It may also be necessary to remove or replace the implant. Scar tissue can form at any time from a few weeks to many years after the implants are inserted.
- Implant shifting or “wrinkling”
- In about 7% of patients (7 out of 100), the implant shifts or settles after the surgery, causing a "wrinkle", "dent" or change of position in the breast implant ("contour irregularity" or “malposition”). These may require more surgery.
Wrinkling is much more common in saline implants, compared with silicone gel-filled implants.
Possible major complications
- Re-operation | Re-hospitalization | Reconstruction failure
- In general, there is a 25% chance of having a major complication after direct to implant reconstruction. That means 25 women out of 100 will need one of the following:
- Re-operation (needing to have another, unexpected surgery)
- Re-hospitalization (needing to be admitted back into the hospital after surgery)
- Reconstruction failure (the reconstruction doesn't work)
You may be at higher risk for complications, based on what you told us about yourself:
- Your BMI (Body Mass Index) is 35 or higher
- You currently smoke
- You are over 60 years old
Learn more about your risk of complications:
Your personalized risk*
Implant reconstruction
- If you have implant-based reconstruction, your risk of a major complication would be 50%.
This means 50 out of 100 women like you have a major complication after implant-based reconstruction.
* This information is only an estimate. Everyone is different, and your risk might be different from what's shown here. Talk with your doctor for more information.
How do other women feel about it?
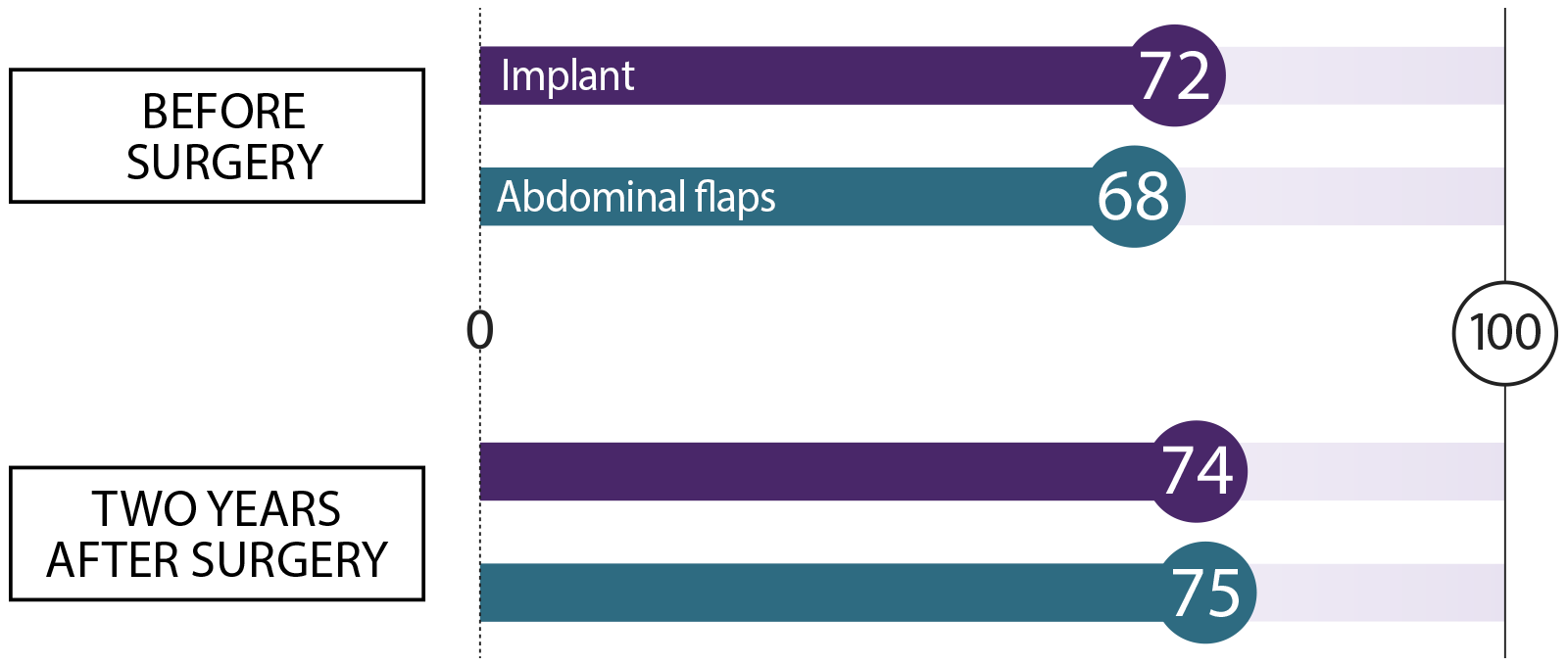
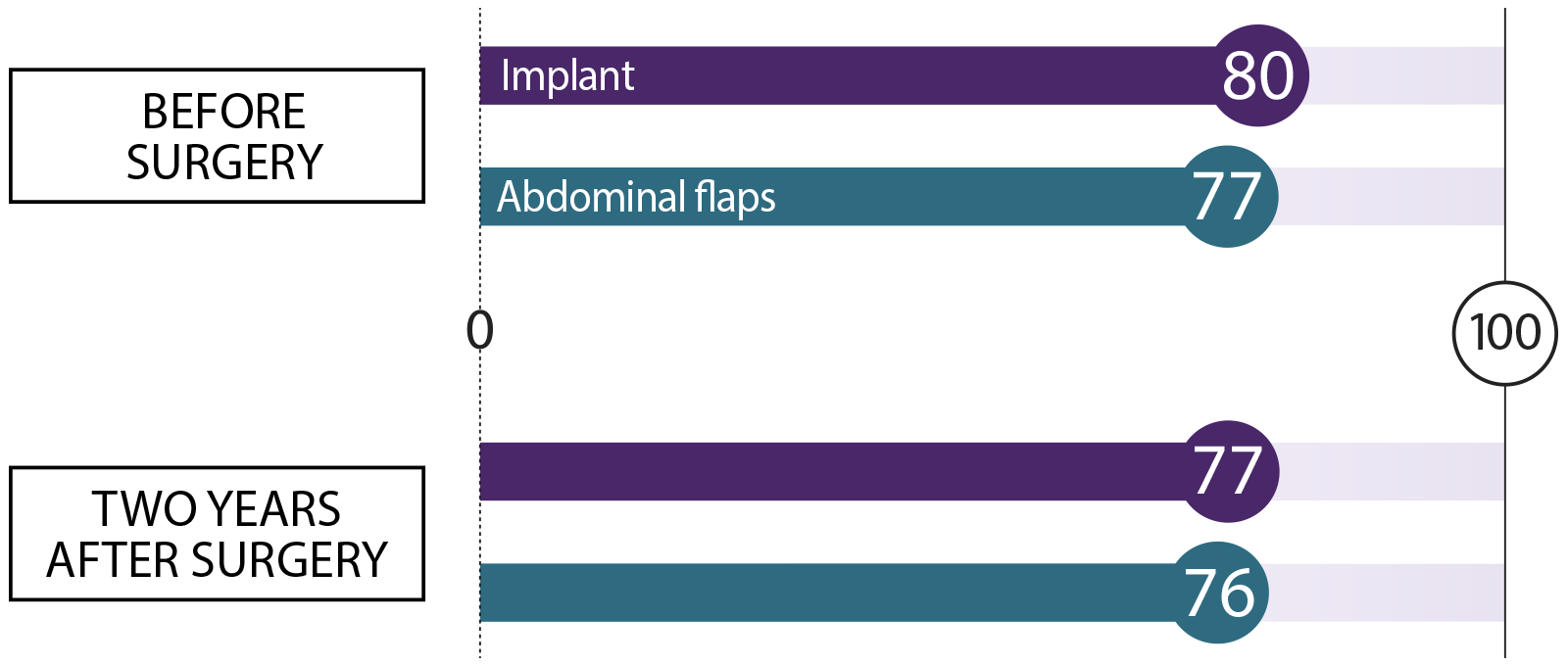
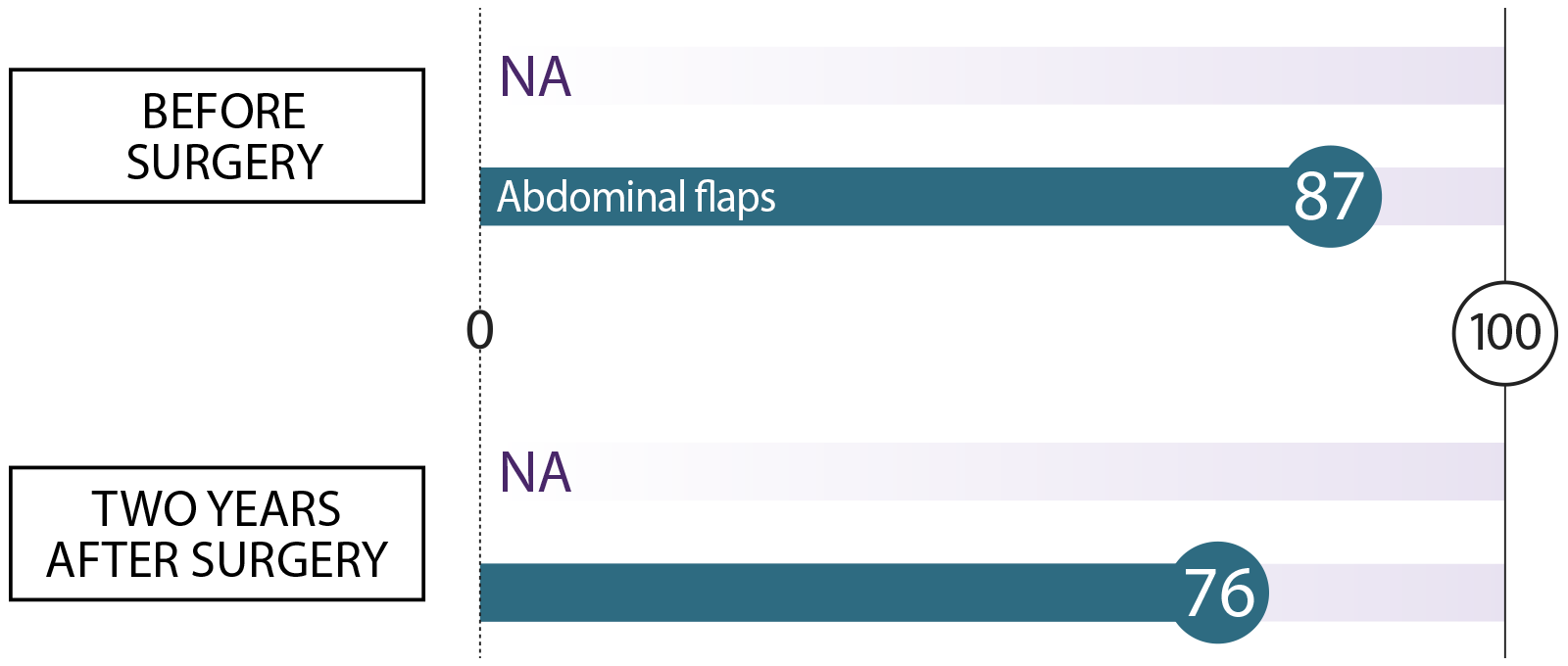
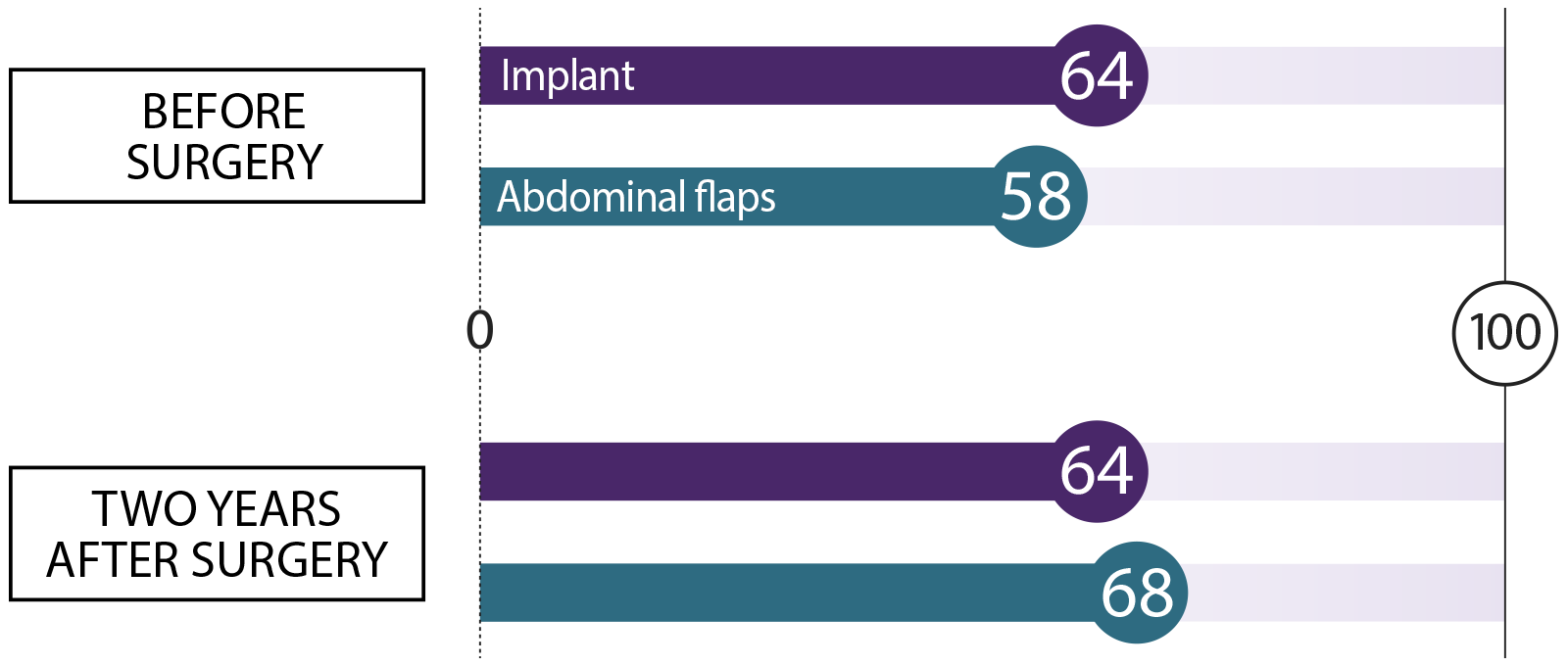
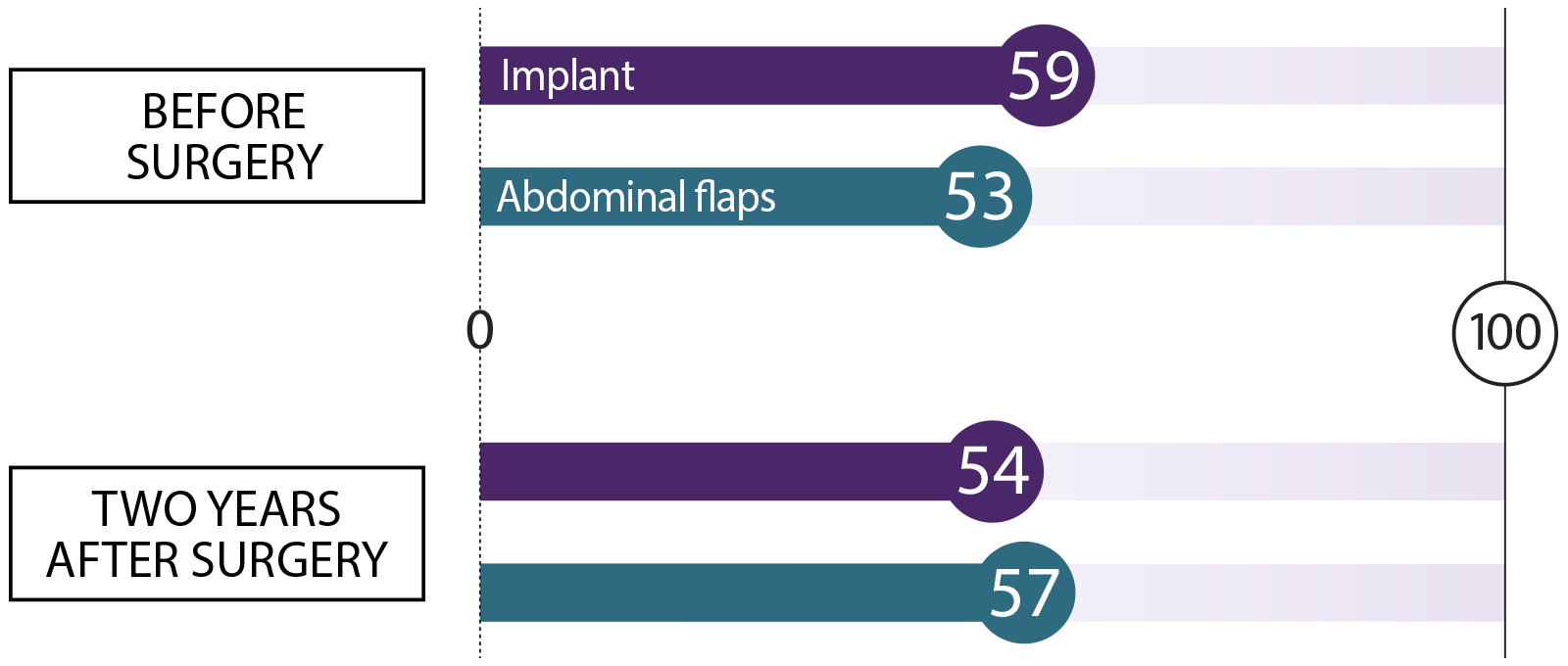
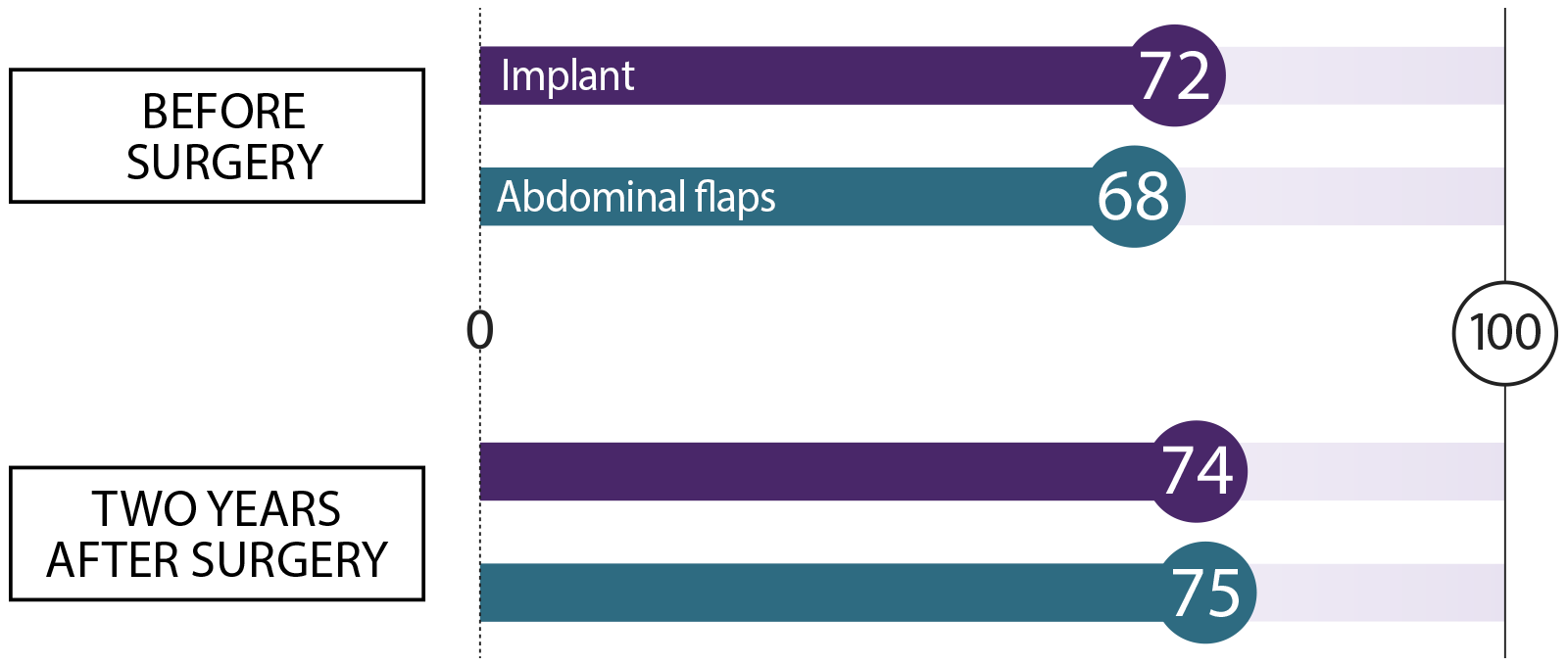
We asked women who had breast reconstruction how they felt before surgery and two years after their procedure. We asked about these topics. Here’s what they said:
Satisfaction with breasts How happy are you with the look and feel of your breasts?
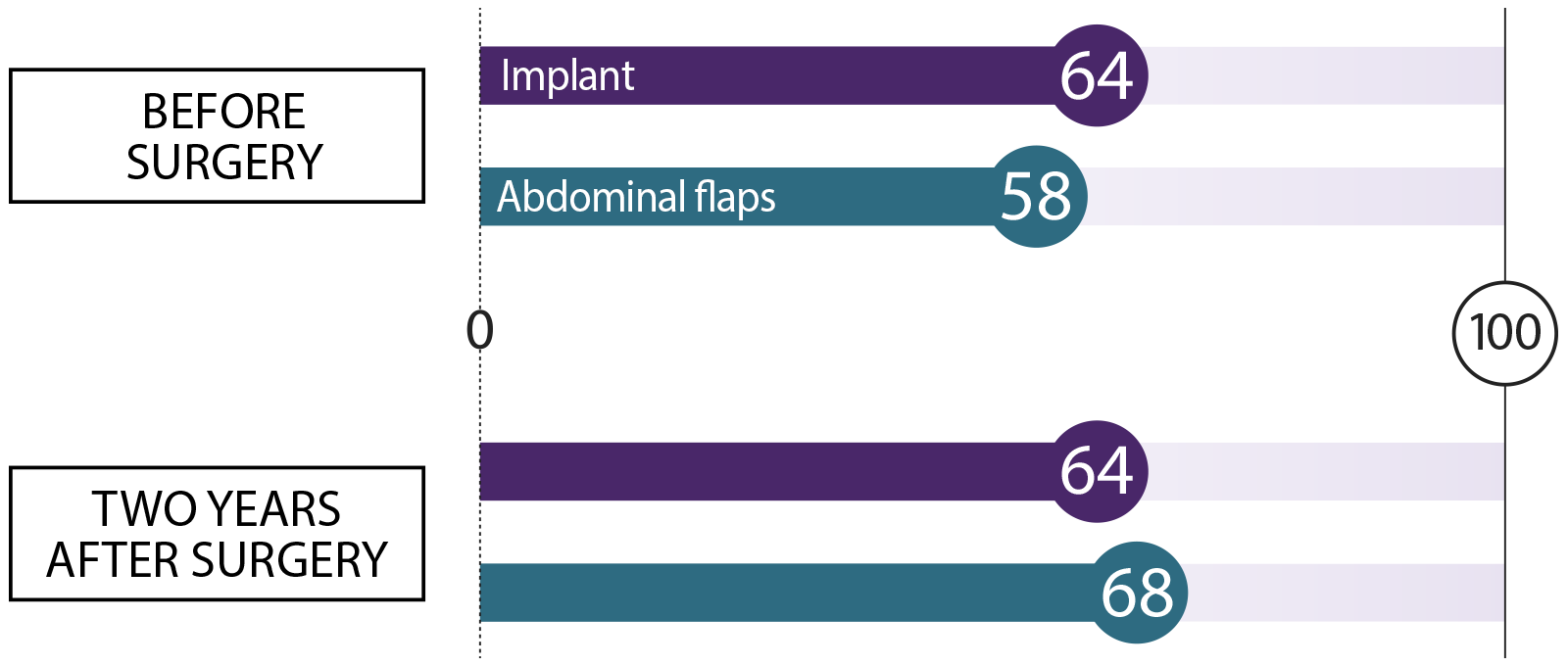 Sexual well-being
Sexual well-being How do you feel about your body as it relates to your sexuality?
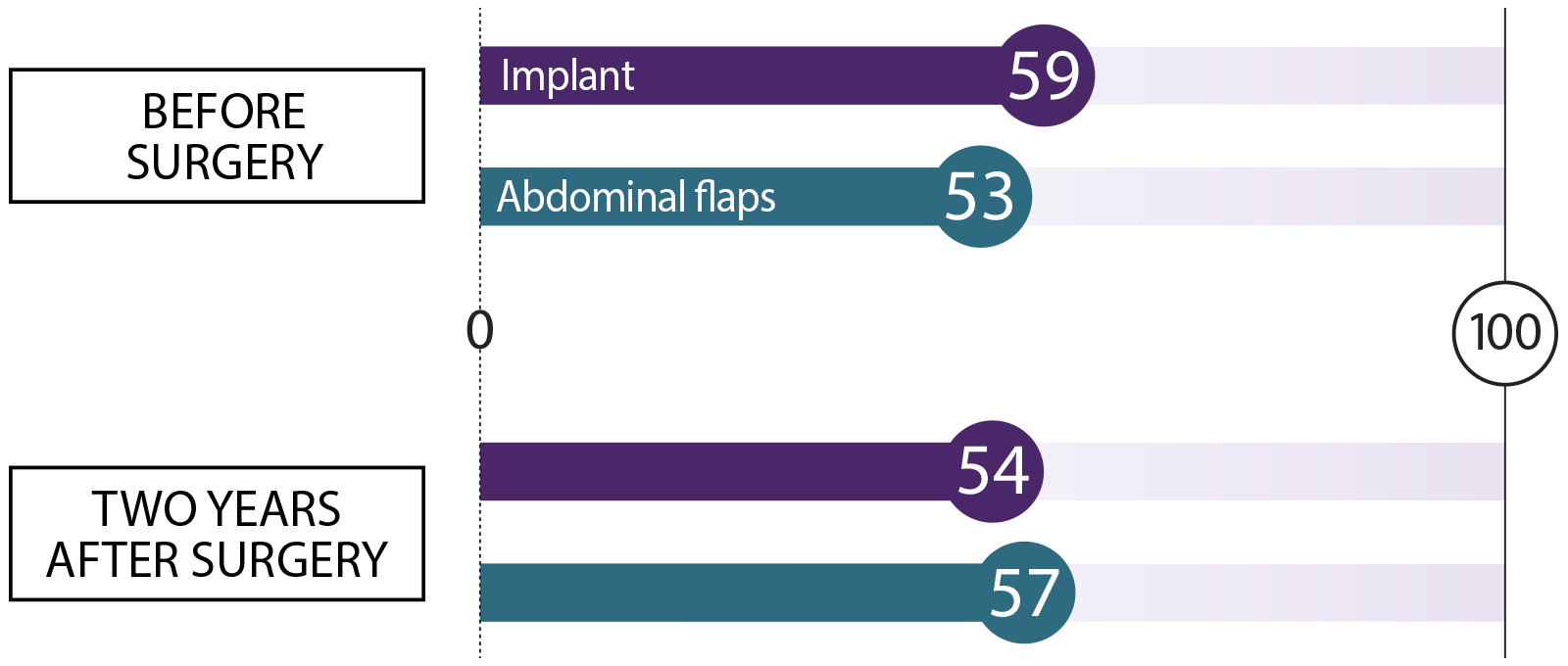 Psychosocial well-being
Psychosocial well-being How do you feel about your body image, and how confident are you in social settings?
 Physical well-being: Chest
Physical well-being: Chest How does your chest feel, physically?
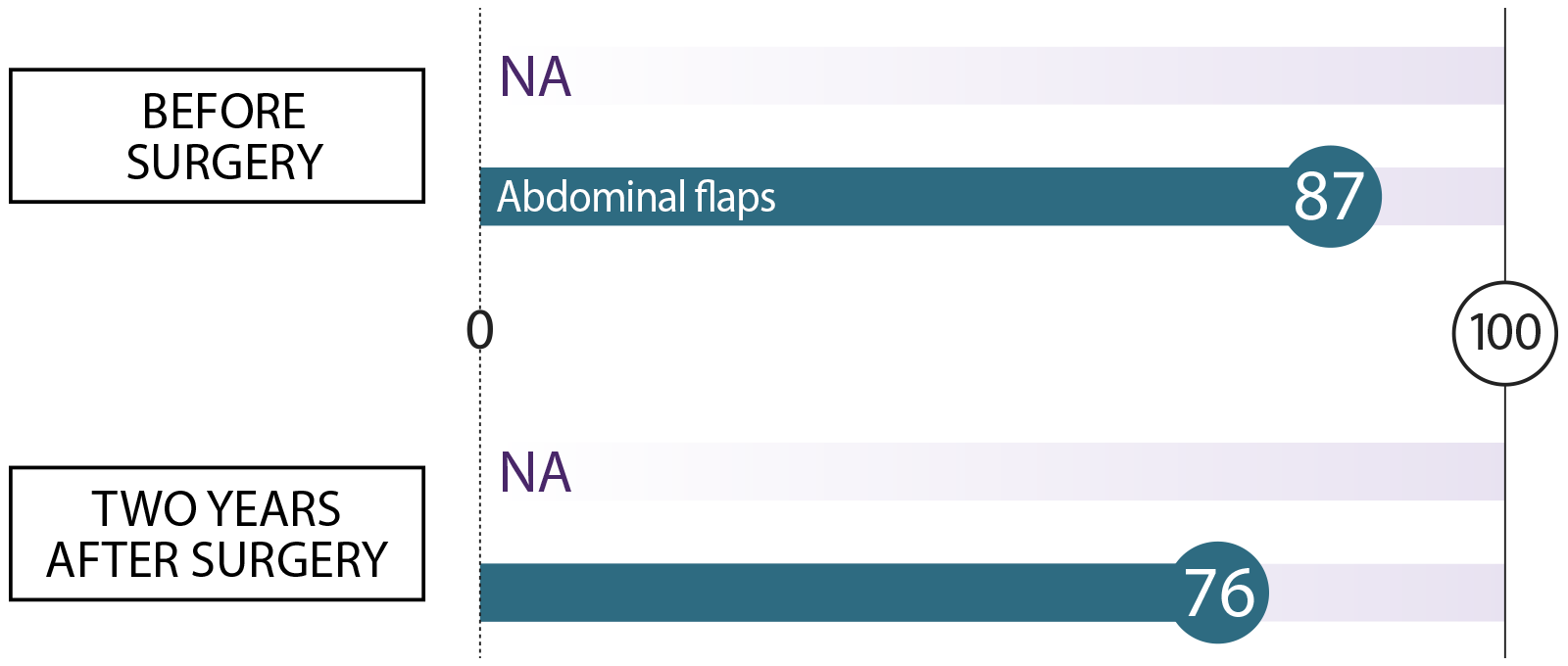
 Physical well-being: Abdomen
Physical well-being: Abdomen How does your abdomen (stomach area) feel, physically?
 Sexual well-being How do you feel about your body as it relates to your sexuality?
Sexual well-being How do you feel about your body as it relates to your sexuality?
 Psychosocial well-being How do you feel about your body image, and how confident are you in social settings?
Psychosocial well-being How do you feel about your body image, and how confident are you in social settings?
 Physical well-being: Chest How does your chest feel, physically?
Physical well-being: Chest How does your chest feel, physically?
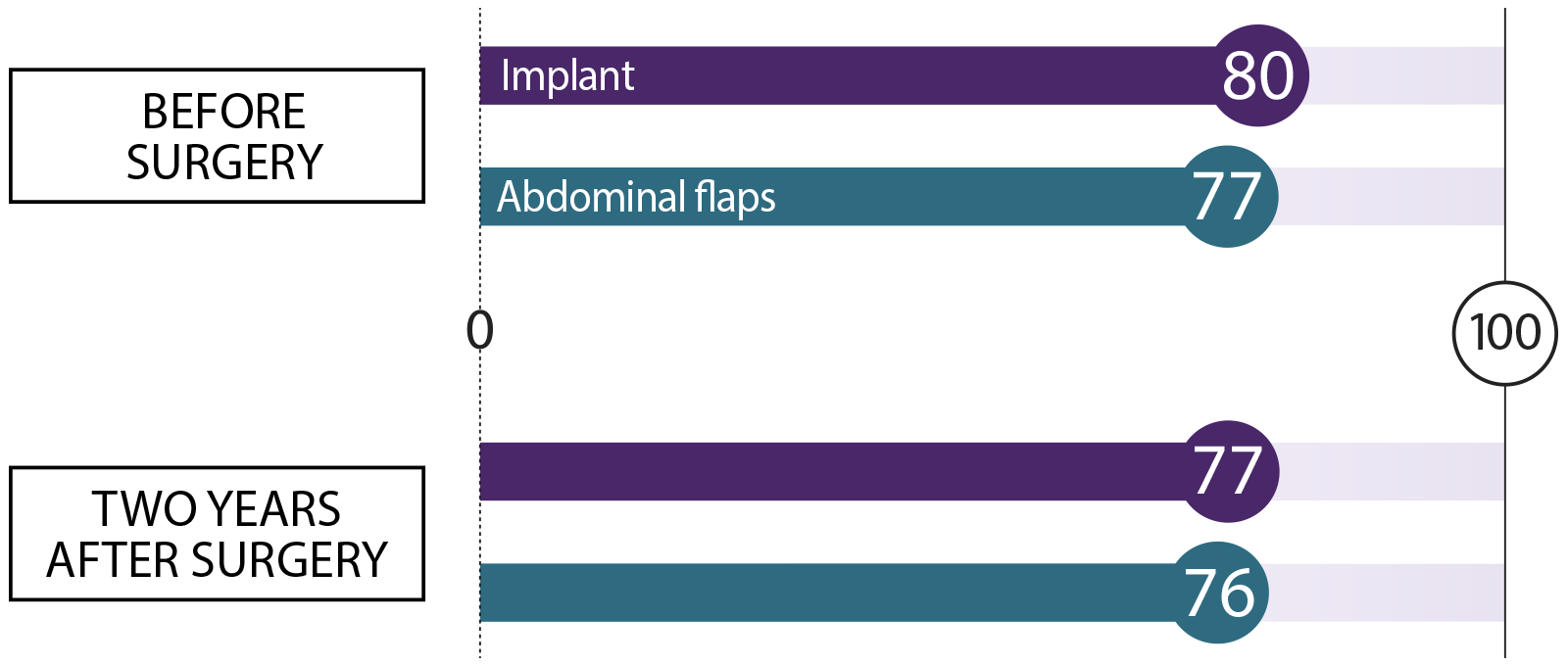 Physical well-being: Abdomen How does your abdomen (stomach area) feel, physically?
Physical well-being: Abdomen How does your abdomen (stomach area) feel, physically?